Automation and Human Expertise Equates to Big Gains
Wuscott lifted this provider's revenue more than 30% in just four months.
Wuscott
7/1/20254 min read
Key Takeaways
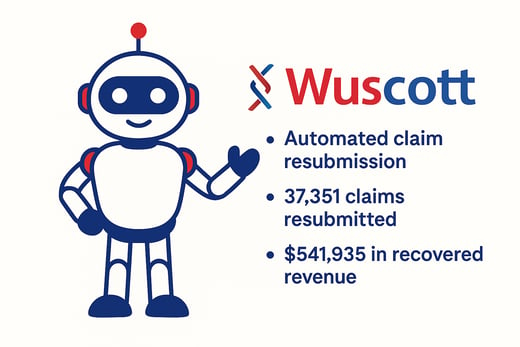
Stagnant Claims: A bot monitored for unacknowledged claims and automatically resubmitted them—resulting in $541,935 in recovered revenue
Bad Insurance Info: Automation paired with manual review corrected 41,747 accessions, generating $486,568 in payments
Aged A/R: Combining bots and human experts, Wuscott worked 60,490 old claims and recovered $2,352,982 in revenue
Human + Bot Synergy: From coding fixes to payer-specific appeals, our dual-path strategy proved critical for long-tail recovery
Background: A national diagnostic lab processing over 7,000 accessions per day was falling drastically short of its revenue projections—by nearly 50%. Despite strong test volumes, collections were lagging due to breakdowns in their revenue cycle management (RCM) processes. Claims were routinely getting “stuck” in the system—never reaching the clearinghouse or payer, and often going unnoticed by staff due to the lab’s massive daily volume.
The client identified Wuscott as the right vendor to assist in identifying problems and deriving solutions. Our process commences with a thorough evaluation of RCM workflows, software, and data, to uncover root causes
Stagnant Claims
With a high throughput client, claims can routinely get “stuck” in the system—never reaching the clearinghouse or payer, and often going unnoticed by staff due to the lab’s massive daily volume. Our team quickly identified that the client’s billing system was not flagging these stagnant claims resulting in idle for weeks—or longer.
Asking the RCM vendor to review its software or address tickets can be daunting and although Wuscott pointed the client towards doing so, Wuscott also deployed an automated resubmission process for this problem. The bot continuously monitors all claims and identifies any that show no acknowledgment activity after 14 days. It then automatically resubmits those claims—without staff intervention—ensuring nothing gets lost in the shuffle.
Between March 1 and July 1, 2025, Wuscott’s bot resubmitted 37,351 claims. Of those, 9,473 resulted in successful payments, generating $541,935 in recovered revenue. The client averages payment after 30 days, so we anticipate many more of these will generate revenue, but for now the numbers associated with an automated process were welcomed by the client:
$14.51 recovered per resubmission
$57.21 per successfully paid accession
Fully automated, zero staff time required
Inaccurate or Missing Information
In the lab industry, insurance information is often incomplete or inaccurate by the time it reaches the billing system—especially for high-volume, ancillary labs that don't collect data at the point of care. This results in tens of thousands of unbilled or denied claims, quietly draining revenue potential.
Wuscott designed a hybrid automation approach combining robotic process automation (RPA) with strategic manual oversight. The bot scans accessions missing valid insurance data, cross-references from previous paid claims, multiple external websites and databases, then applies logic to identify the most likely insurance and correct bad or missing information. For edge cases, manual intervention fills the gap—turning “unbillable” into paid.
$7.88 per accession corrected
$79.45 per successful payment
Hybrid automation reduces denials and boosts clean claim rates


Accumulating Accounts Receivable
With more than $100 million in aging accounts receivable—and tens of thousands of accessions over 60 days old—this client was sitting on a massive backlog of unpaid claims. Many dated as far back as January 2024, long forgotten or assumed uncollectable. Automation alone couldn’t fix it all. This was a situation that demanded both expert human oversight and intelligent automation.
Wuscott designed a dual-path recovery strategy. Our automation bots scanned and triaged old claims, flagging those eligible for resubmission, correction, or appeal. In parallel, our RCM specialists reviewed claims requiring nuanced action—missing modifiers, improper diagnosis codes, or denials that required payer-specific appeals.
Key workflows included code corrections for medical necessity and bundling edits, intelligent appeal generation, and automated and manual rejection handling
$38.89 per claim worked
$137.33 per paid claim
Historic AR recovery without exhausting internal teams
Lessons Learned
Stagnant Claims: A bot monitored for unacknowledged claims and automatically resubmitted them—resulting in $541,935 in recovered revenue
Bad Insurance Info: Automation paired with manual review corrected 41,747 accessions, generating $486,568 in payments
Aged A/R: Combining bots and human experts, Wuscott worked 60,490 old claims and recovered $2,352,982 in revenue
Human + Bot Synergy: From coding fixes to payer-specific appeals, our dual-path strategy proved critical for long-tail recovery
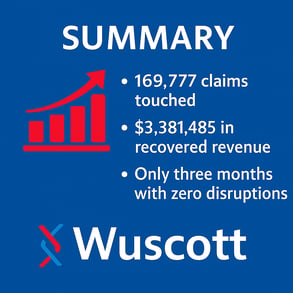
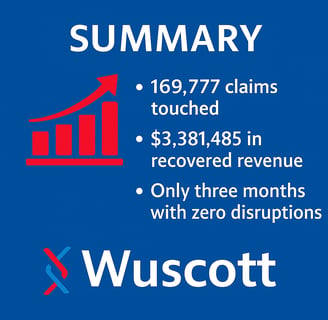
Total Value Delivered (Mar–Jul 2025): 169,777 claims touched → $3,381,485 in recovered revenue
Wuscott’s approach simply involves data analysis to identify gaps, automate wherever possible, intervene when necessary, and deliver measurable returns with minimal disruptions. Wuscott was engaged by a large diagnostic lab facing widespread revenue leakage across its revenue cycle operations. With over 7,000 accessions per day and $100M+ in aging A/R, the lab had strong test volume but weak collections—falling nearly 35% below projections.

What Can Automation do for You?


